HDG #032: Ten (10) health plan concepts to know
Last week we explored key stakeholders across the healthcare ecosystem, and this week we’re zeroing in on one of my favorites: health plans.
This post will pave the way for further posts where we deep dive into many of the calculations and data concepts that are largely used by health plans, but that every person working in healthtech or care delivery should become familiar with.
For those unfamiliar, a health plan is essentially a type of insurance coverage that “pays” for medical and surgical expenses incurred by the insured. Health plans can either reimburse the insured for expenses incurred from illness or injury, or pay the care provider directly. They are a critical component of healthcare systems in many countries, especially in settings where healthcare costs can be prohibitively expensive without insurance coverage.
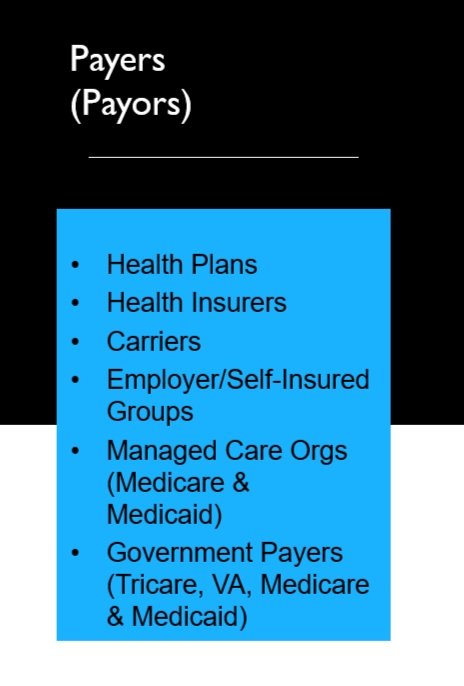
You may also see them by different names, all with slight nuances to them. The list below shows some examples and types. This list is not comprehensive. I like to think of it as an entity responsible for financially covering the care of (and in an ideal world, managing the care of) an individual (member) or population (group).
Understanding how health plans operate and use/analyze data is crucial for both healthtech operators and for providers considering taking on some of the risk (or shared responsibilities). Luckily, there are some commonalities across plans in how they talk about operations and metrics that they’re often looking at.
Here are 10 health plan concepts to know:
PMPM (Per Member Per Month): A fundamental metric in health plan finance, PMPM measures the average expenditure on healthcare services for each member every month. For example, a PMPM of $500 in one population might reflect higher healthcare needs (or costs) compared to a lower PMPM in a different group. Similarly, costs of services are often compared on a PMPM basis. In fact, I wrote an article dedicated to PMPM and why I think it is the most important metric in healthcare, with some examples of how to calculate it and how it impacts more stakeholders than just payers.
Per 1000 Metrics: These are standardized measures to compare healthcare service utilization across different populations. For instance, measuring ER visits per every 1000 members helps identify which population groups use emergency services more frequently and why. From a health plan perspective, the number of events/admissions/utilization/scripts/procedures/etc. per 1000 is typically represented as an annualized value.
One quick formula I like because you can compute it on your calculator in this order, without worrying about the order of functions or denominators, is:
# of [events] ÷ # of member months in the period * 12000
Case Management: Case management in a health plan context primarily focuses on individual patients, particularly those with complex medical needs, chronic conditions, or high costs. Among other things, the goal is to optimize health outcomes via managing members’ healthcare journey, conducting and monitoring health risk assessments, and helping members navigate the system via care coordination and disease management programs. Data in case management can track the effectiveness of interventions, like how coordinated care reduces hospital readmissions for chronic heart failure patients, as an example. More and more we are also starting to see more social needs addressed.
Utilization Management (UM): This involves evaluating the medical necessity, appropriateness, and efficiency of the use of healthcare services, procedures, and facilities from the health plan’s perspective. Providers/hospitals also have similar processes on their side, but from the health plan’s side, nurses and doctors review claims/cases, documentation, medical histories, and care requests to approve/deny care based on medical necessity and policy. Not all services require authorization before they’re covered (“prior auth”) but many do. You also see “concurrent reviews” as the clinical team monitors and evaluates the need for ongoing care, such as prolonged inpatient hospital stays or extensive treatment plans, to determine if they continue to be appropriate and necessary. For much of this work, they rely on clinical knowledge and industry-standard clinical/care guidelines. Data from UM could highlight trends like increased MRI usage, prompting health plans to investigate whether these tests are medically necessary. UM has faced criticism for potentially restricting patient access to care and increasing the administrative burden on healthcare providers. For instance, UnitedHealth even came under suit recently at the allegation of using an AI algorithm to systematically deny claims without review.
Paid/Allowed/Billed Amounts: These financial terms reflect different aspects of healthcare billing. 'Billed' is the amount charged by providers (i.e. what is on their Chargemaster as what they “charge” for procedures), 'allowed' is what the insurance plan agrees to cover and is permitted to be covered based on the policy and benefits of the plan, and 'paid' is the actual amount paid out. Analyzing discrepancies among these can reveal insights into provider pricing strategies and insurance coverage limitations. Using the wrong field in an analysis can be absolutely catastrophic. There are also other dollar fields, such as deductibles, copay, coinsurance, and more, but these are the 3 most commonly used in analysis from my experience.
ACO (Accountable Care Organization): This is a bit of a chameleon concept since it is important on both the plan and provider side. I grouped it here with health plans because of the nature of how these organizations are mobilizing and collaborating to take on more responsibility for the care of an individual member or group (the definition I used earlier). ACOs are groups of healthcare providers who agree to share responsibility for the quality, cost, and overall care of patients. ACOs may operate under a payment model that rewards providers more for meeting specific benchmarks for quality and efficiency, such as within the Medicare Shared Savings Program. You may have also heard of a similar but different term, Clinically Integrated Network (CIN). A CIN is a collection of healthcare providers, such as physicians and hospitals, that come together to improve patient care and reduce costs through enhanced coordination and collaboration. The focus of a CIN is on clinical integration to improve overall care quality, patient outcomes, and cost efficiencies across all payers and patient populations, not just Medicare. CINs operate under various payment models, including fee-for-service and value-based care contracts. They focus on creating a cohesive, collaborative environment where data and best practices are shared to improve care quality while seeking to retain provider independence in many cases. In either case, data analysis here might focus on how ACOs manage to reduce unnecessary hospitalizations while improving care quality.
Self-funded vs. Fully-insured: In the educational video that I shared last week, Navigating the healthcare ecosystem, I talk about how the money flows in healthcare, often from an individual person to their employer, to a payer-type entity to actually administer the program. But what you might now know is in some cases, your employer may actually be the one bearing the risk (aka paying for all the healthcare costs) for its employees—again, like the definition I used of a payer earlier in the article. The scenario where the employer assumes the financial risk for providing healthcare benefits to its employees is called a “self-funded” plan (though they still may contract with a Cigna or the likes as an ASO (Administrative Services Only) to handle administration like processing claims, member services, and provider network management, but not bear risk. We typically see this with much larger employers with the financial resources and many employees. Most employer plans fall into the more traditional “fully insured.” In a fully insured health plan, the employer pays a fixed premium to an insurance company, which then assumes the financial risk for paying all healthcare claims. Premiums are determined based on factors like the number of employees and projected healthcare costs. In the latter arrangement, the employer may have less control over their healthcare costs and benefits design than in the former, and both come with a slew of other pros/cons and conversations revolving around employee healthcare costs (if interested, I encourage you to follow Chris Deacon, Esq).
COB (Coordination of Benefits) & Duals: COB is a process used by health insurance companies to determine the payment responsibilities when a patient is covered by more than one health insurance plan. It ensures that the combined payment from all plans does not exceed the total amount of the claim. We often see this happen when a member has one insurer through their employer, and a different one through their spouse. Or they may have been in an accident so an auto insurer or workman’s compensation is going to pay for some of the medical costs. "Duals" or "Dual Eligible" refers to individuals who are specifically covered by both a combination of Medicare and Medicaid benefits. This group typically includes older adults and people with disabilities who meet specific income and asset criteria, and often reflect very high-needs complex cases. In the latter cases, it is especially important to pay attention to a member showing up “twice” in the claims data (one under their Medicaid number, and another under their Medicare number), or even in two different and separate “cases” or files in the case management software, etc.
MLR (Medical Loss Ratio): MLR measures the percentage of premium dollars an insurance company spends on providing healthcare services (claims) and activities to improve healthcare quality. This ratio indicates the percentage of premiums spent on patient care and quality improvement versus administrative costs. For instance, an MLR of 85% means 85% of premium revenues are used for patient care, a crucial indicator of a health plan’s focus on patient welfare. There are rules and regs about what can count as “administrative” versus “medical” expenses, as well as minimum MLR requirements set forth in the past to promote accountability and value for healthcare consumers.
Contribution Margin: This one is a bit lesser known but one of my favorites, and I’ve seen it sliced a couple of different ways. In general, it is meant to show the profitability of a specific service, line of business, or other sub-group. Said another way, to what extent the service, line of business, or other sub-group is “contributing” to profit (or loss). Health plans use the contribution margin to assess the financial viability and profitability of different services or member segments. It helps in determining which services are more beneficial to continue or expand, and which to focus more energy on managing or deploying new programs. For instance, a high contribution margin for a digital therapy app compared to traditional therapy sessions might favor a shift towards more cost-effective digital health solutions. On the other side of profit, I’ve also seen this used to show which lines are loss leaders, and even WITHIN one group (say, Medicaid) which sub-groups are “carrying” the line and which sub-groups are perpetually in the red.
Why all of this matters in data
Each of these concepts plays a vital role in understanding the financial and operational aspects of health plans. By applying data analytics in these areas, health professionals can make more informed decisions, identify trends, and spot opportunities for improvement.
More importantly, even if you are not working at a health plan and sit somewhere else in the ecosystem: these are terms that will make their way into conversations about contracting, payments, and services as you’re working with health plans—whether you’re a provider, vendor, or other stakeholder. These are concepts and facets of business operations that payers are living and breathing on a daily basis, therefore influencing how they talk to you about their plights and what kind of solutions or support they’re looking for.
. . .
Actionable Idea of the Week:
This week, I encourage you to learn a little more about the payer world:
Learn more about PMPM in our article about why it’s the most important metric in healthcare
Review our Guide to CMS-1500 Professional Claim Fields
Bonus: if you like bite-sized lists like these, check out our tiny glossary of healthcare terms to know
. . .
Having knowledge of these concepts is essential in our current healthcare landscape as more providers look to take on risk or delegated services like case management/care coordination, as more “payviders” appear in the world, and as “value-based care” conversations continue to… be around. For analysts, they serve as the foundation of health plan data, leading to strategic insights and impactful innovations in healthcare. And we’re just getting started breaking some of these down!
More next week,
-Stefany
P.S. I recently revised some of my content based on data about my readership. That said, topics on a weekly basis may range from introductory to more advanced and complex, or from commonplace topics to very niche challenges I’m seeing in my world. If you have any ideas, suggestions, feedback, or requests for specific topics, I’m always open. Hit reply and let me know!!